|
Chapter 12 : AsystoleAsystole is associated with the absence of cardiac electrical activity, contraction of the heart muscle, and cardiac output. "Flatline" is a term used for no electrical activity seen on the ECG. However, "flatline" can result from other causes such as:
Asystole ACLS Training Video:
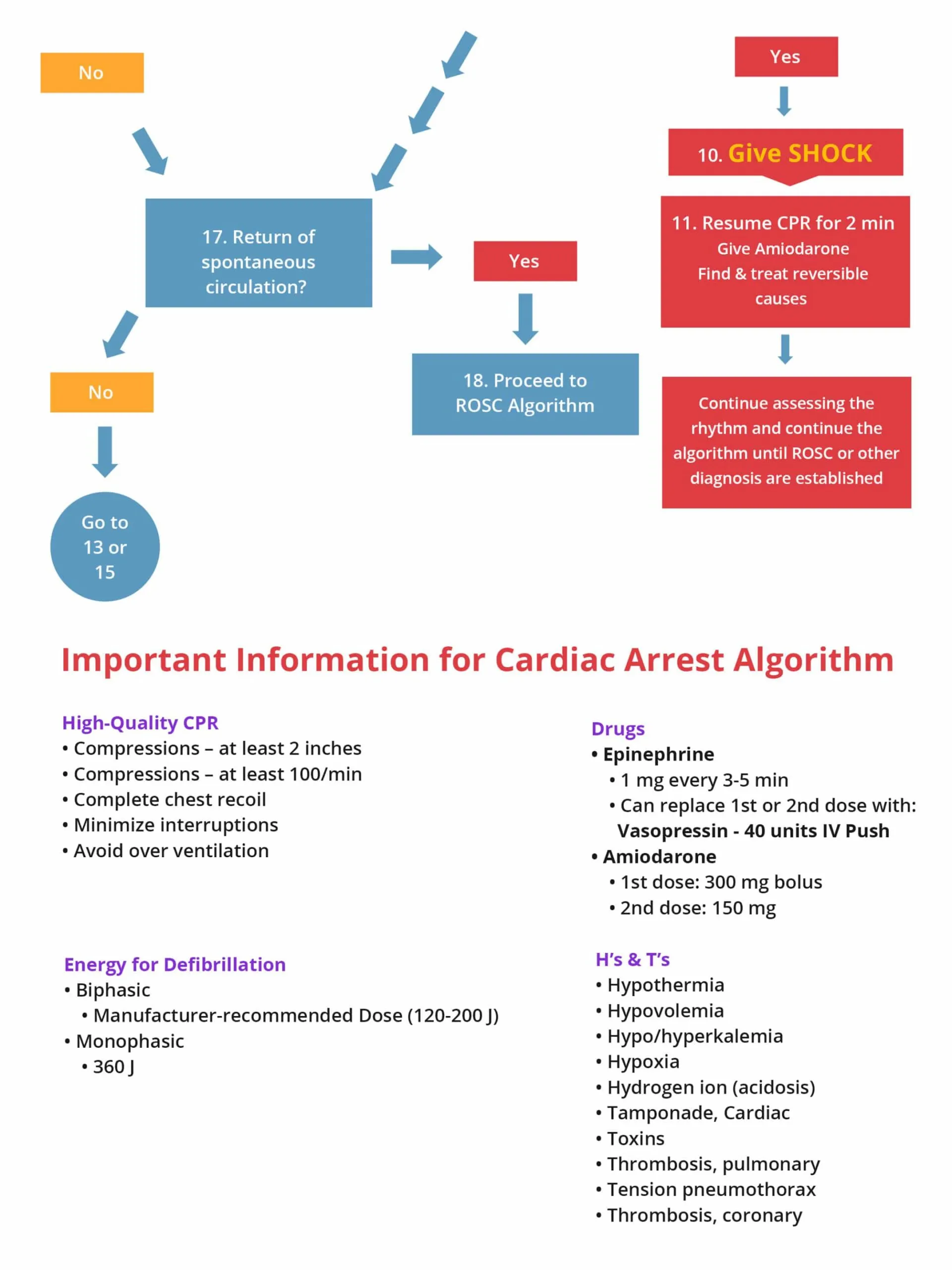
Asystole can be caused by many factors and are represented as H’s and T’s:
Scenario: You are a paramedic and arrive on the scene. A man is lying on the floor unconscious and the neighbor tells you that she saw the man collapse as he was unlocking his front door. Assessment:
Interventions:
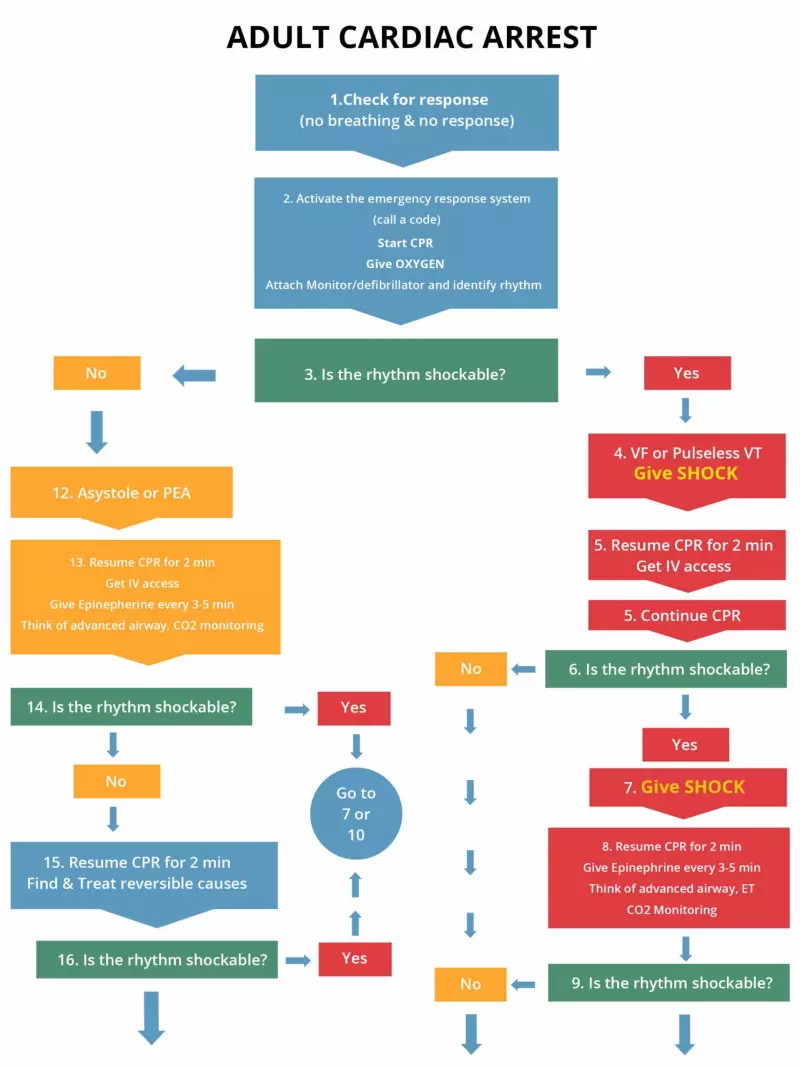
Management: AT the hospital initiate the cardiac arrest algorithm on the right if the patient still has no pulse and does not respond to BLS. Get a code team in place.
The following is an algorithm shows management of cardiac arrest due to a flat line situation or asystole/PEA (left side of chart)
Note: When conducting the BLS and ACLS survey on a patient with asystole, there may be times when you should hold resuscitative efforts; those include:
Learning Outcomes:You have completed Chapter XII. Now you should be able to:
|
||||||||||||
Asystole is associated with the absence of cardiac electrical activity, contraction of the heart muscle, and cardiac output. "Flatline" is a term used for no electrical activity seen on the ECG. However, "flatline" can result from other causes such as:
| H’s | T’s |
| Hypovolemia – Decreased blood volume | Tension pneumothorax – air in the pleural space around the lung (lung collapses) |
| Hypoxia- decreased partial pressure of oxygen in blood | Tamponade – compression of the heart produced by excess fluid surrounding the heart |
| Hydrogen ion (acidosis) – Increase in the concentration of H ions in blood | Toxins – poisonous substances |
| Hyper-/hypokalemia –abnormally high or low potassium concentration in the blood | Thromobosis (pulmonary) – formation of a blood clot which blocks a blood vessel in lungs |
| Hypothermia – body temperature less than 30 degrees C (86 degrees F) | Thrombosis (coronary) –formation of a blood clot which blocks a blood vessel in heart |
Scenario: You are a paramedic and arrive on the scene. A man is lying on the floor unconscious and the neighbor tells you that she saw the man collapse as he was unlocking his front door.
Assessment:
Interventions:
Management: AT the hospital initiate the cardiac arrest algorithm on the right if the patient still has no pulse and does not respond to BLS. Get a code team in place.
Once IV/IO access is obtained give the following drugs:
The following is an algorithm shows management of cardiac arrest due to a flat line situation or asystole/PEA (left side of chart)
Note: When conducting the BLS and ACLS survey on a patient with asystole, there may be times when you should hold resuscitative efforts; those include:
You have completed Chapter XII. Now you should be able to: