|
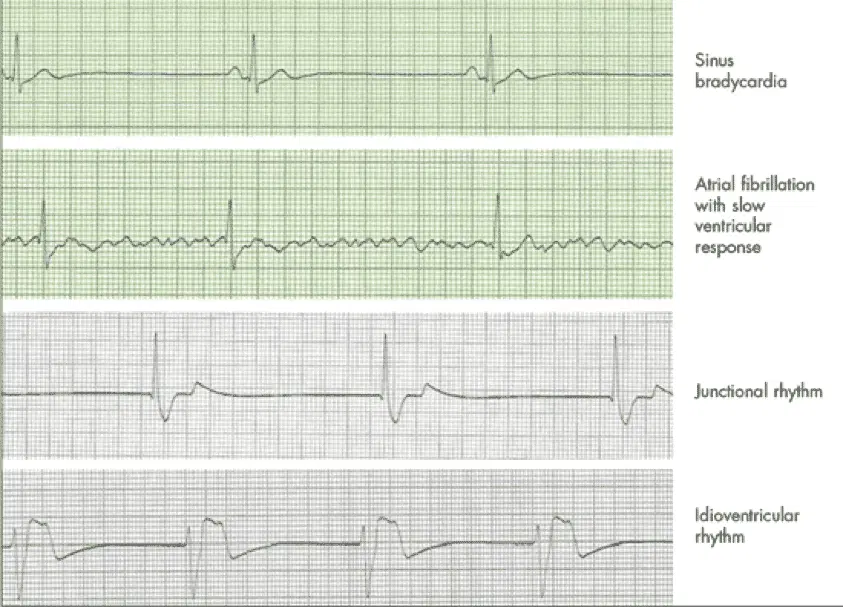
Chapter 11 : Pulseless Electrical ActivityWhen a patient goes into cardiac arrest, their heart stops beating and they don’t have a pulse and that is when Pulseless electrical activity (PEA) or cardiac contraction occurs. If you eliminate the main cause of PEA arrest, patients with PEA can survive. Even though the heart is producing organized electrical activity, no mechanical activity is produced. There will be no contractions of the cardiac muscles. Any organized rhyme without a pulse is PEA (except VF, VT and asystole) and includes: idioventricular rhythms, ventricular escape rhythms, post-defibrillation idioventricular rhythms, and Bradyasystolic rhythms. ACLS Pulse-less Electrical Activity Video:
PEA can be caused by many factors and are represented as H’s and T’s:
Scenario: You are the physician on duty and are called to the ER to see a patient who was involved in a motorcycle accident and is now unresponsive. PEA Assessment:
PEA Interventions:
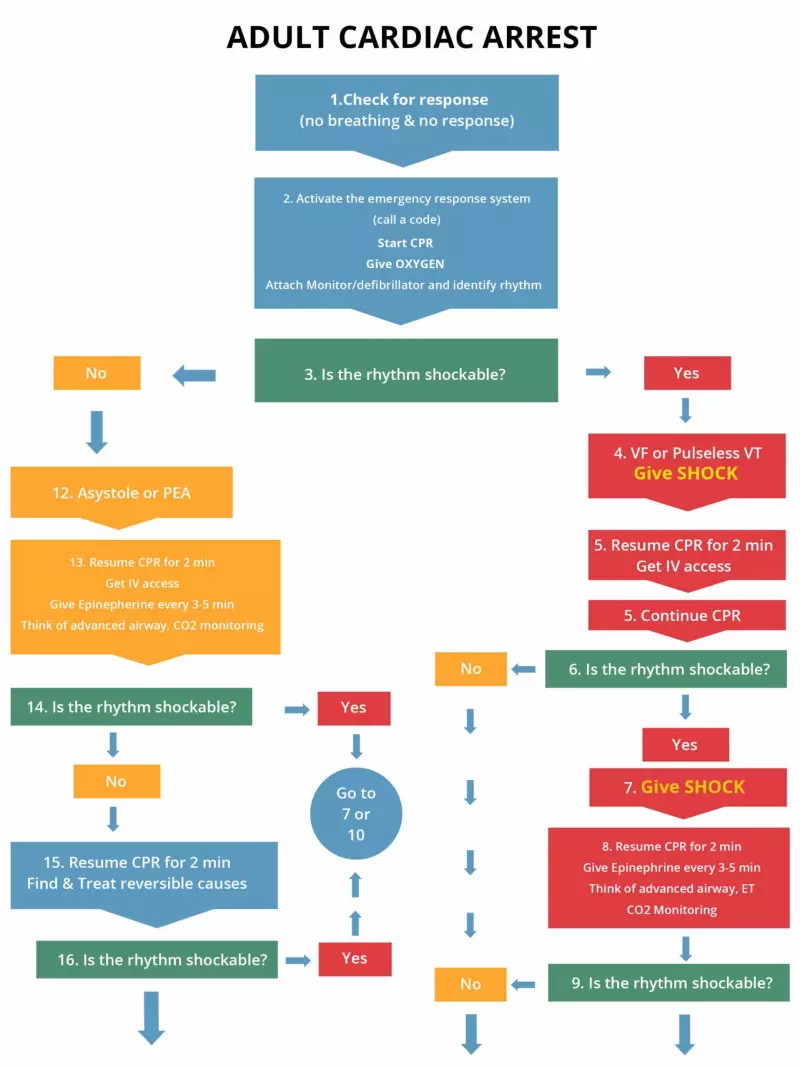
The following is an algorithm shows management of cardiac arrest due to asystole/PEA (left side of chart)
To ensure the best outcome for PEA it is vital to have uninterrupted, high quality CPR and to quickly figure out the reversible causes. Learning Outcomes:You have completed Chapter XI. Now you should be able to:
|
||||||||||||
When a patient goes into cardiac arrest, their heart stops beating and they don’t have a pulse and that is when Pulseless electrical activity (PEA) or cardiac contraction occurs. If you eliminate the main cause of PEA arrest, patients with PEA can survive. Even though the heart is producing organized electrical activity, no mechanical activity is produced. There will be no contractions of the cardiac muscles. Any organized rhyme without a pulse is PEA (except VF, VT and asystole) and includes: idioventricular rhythms, ventricular escape rhythms, post-defibrillation idioventricular rhythms, and Bradyasystolic rhythms.
| H’s | T’s |
| Hypovolemia – Decreased blood volume | Tension pneumothorax – air in the pleural space around the lung (lung collapses) |
| Hypoxia- decreased partial pressure of oxygen in blood | Tamponade – compression of the heart produced by excess fluid surrounding the heart |
| Hydrogen ion (acidosis) – Increase in the concentration of H ions in blood | Toxins – poisonous substances |
| Hyper-/hypokalemia –abnormally high or low potassium concentration in the blood | Thromobosis (pulmonary) – formation of a blood clot which blocks a blood vessel in lungs |
| Hypothermia – core temp is less than 96.8 F, and severe is less than 86 F | Thrombosis (coronary) –formation of a blood clot which blocks a blood vessel in heart |
Scenario: You are the physician on duty and are called to the ER to see a patient who was involved in a motorcycle accident and is now unresponsive.
Once IV/IO access is obtained give the following drugs:
The following is an algorithm shows management of cardiac arrest due to asystole/PEA (left side of chart)
To ensure the best outcome for PEA it is vital to have uninterrupted, high quality CPR and to quickly figure out the reversible causes.
You have completed Chapter XI. Now you should be able to: