Chapter 4 : Bradyarrhythmias and TachyarrhythmiasCardiac dysrhythmia or arrhythmias are caused by abnormalities in the electrical activity of the heart and can be classified as bradyarrhythmias, tachyarrhythmias or pulseless arrest. They are associated with an increased heart failure. Cardiac arrhythmias are accelerated, irregular or slow heart rates caused by abnormalities in the myocardium. BradyarrhythmiasBradyarrhythmias are the most common arrhythmias in children and usually presents with hypoxemia, hypotension and acidosis. Bradycardia is a heart rate which is slower than the normal for the age of the child; usually less than 60 bpm is indicative of bradycardia and immediate CPR should be initiated.
PALS by American HealthCare Academy Video:There are 5 examples of bradyarrthmias that are seen in children:
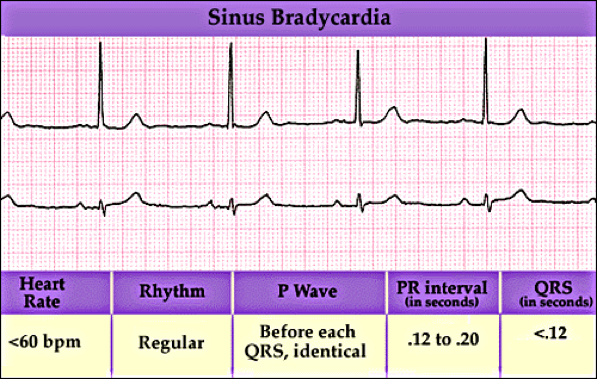
PALS by American HealthCare Academy Video:Sinus Node Arrest/Sick Sinus SyndromeSinus node arrest/sick sinus syndrome is associated with abnormal heart rhythms due to malfunction of the sinus node. These may include atrial, junctional and idioventricular escape rhythms. Sinus BradycardiaSinus bradycardia starts in the SA node with decreased rate (<60 beats/min). It develops due to decreased metabolic demand and may be caused by hypoxia, poisoning, hypoglycemia, or hypothyroidism.
First Degree AV Block First degree AV block is when the PR interval is prolonged (> 0.20 seconds) and impulse from atria to ventricles through the AV node is delayed. There usually are no symptoms associated with first-degree AV block.
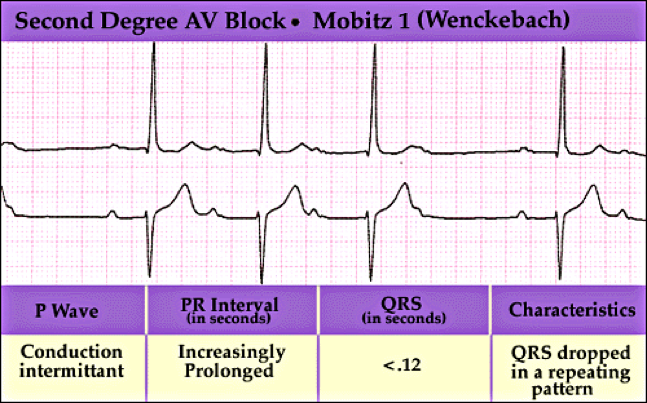
Second Degree AV Block Type I 2nd Degree AV block type I (Wenckebach-Mobitz I) is when the PR intervals are prolonged, R-R intervals are shortened and finally one beat drops. Symptoms may include dizziness, but usually not seen.
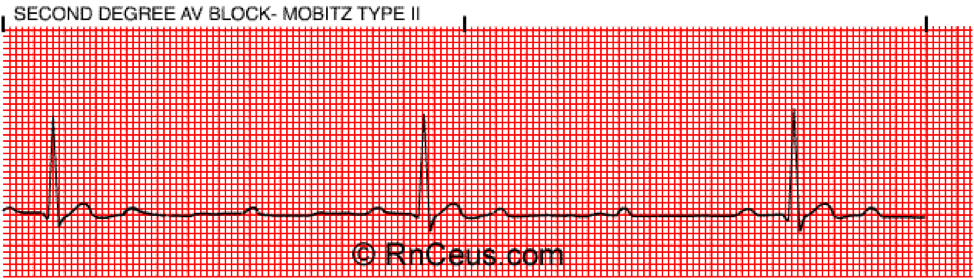
Second Degree AV Block Type II 2nd degree AV block Type II (Mobitz II) is when there is no change in the PR interval and then a beat will drop randomly. Symptoms may include irregular heart bear, presyncope or syncope.
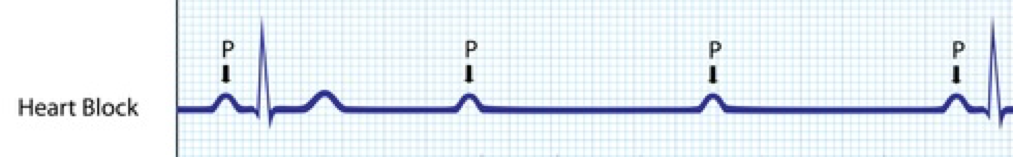
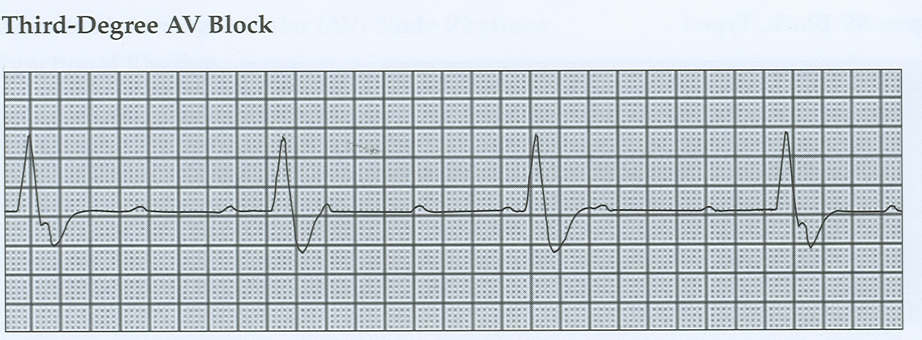
Third Degree AV Block 3rd degree Av block is a complete heart block where the P wave and QRS complexes are not connected. Impulse conducted in the atrium does not progress to the ventricles. There is no communication between the atrium and the ventricles. Symptoms include fatigue, presyncope or syncope.
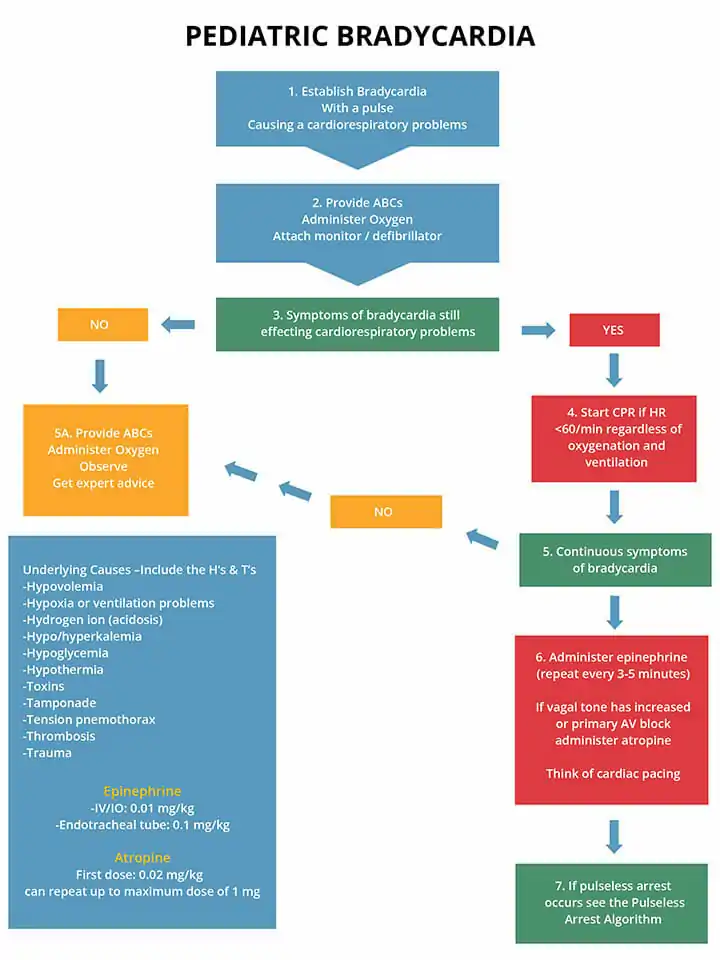
Management of BradyarrhythmiasProper management of bradyarrhythmia includes managing for heart rate and respiratory distress or failure. The following are steps in the treatment of bradycardia:
TachyarrhythmiasTachyarrhythmias are considered fast abnormal rhythms, which originate from the atria or ventricles. Tachycardia is a heart rate which is faster than the normal for the age of the child; and immediate CPR should be initiated.
The following are examples of tachycardia:
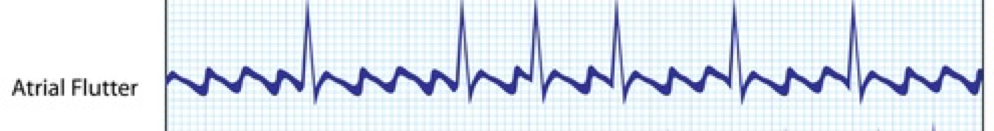
Atrial FlutterAtrial flutter is abnormal heart rhythm causing fast irregular heartbeat. Usually occurs in the atria of the heart and is uncommon in children. Some causes of atrial flutter include: hypertension, ischemia, cardiomyopathy, and abnormal heart valve.
Sinus TachycardiaSinus tachycardia is when the rate of impulse from the SA node is elevated than normal for age. Heart rate <220 bpm in infants, <180 bpm in children, P wave is normal, PR interval is constant, and R-R interval is variable. Some causes of ST include: hypoxia, hypovolemia, fever, poison, metabolic stress, trauma, pain, anxiety, toxicity, and anemia.
SVTSupraventricular Tachycardia (SVT) is a rapid heartbeat that starts right above the ventricles. SVT is the most common cause of tachyarrhythmia in infants causing cardiac issues. Heart rate >220 bpm in infants, >180bpm in children, p wave is abnormal; R-R interval is constant. Some causes of SVT include: AV nodal reentry, ectopic atrial focus, and accessory pathway entry.
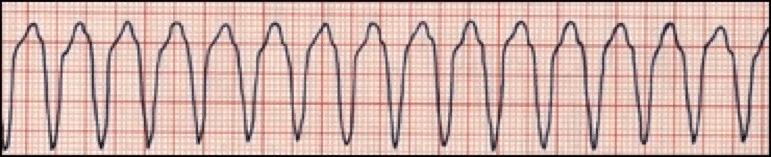
Ventricular Tachycardia (VT)Ventricular tachycardia (VT) starts in the ventricles and is uncommon in children, and the heart rate is regular and at least 120 bpm. VT with pulse can cause the heart rate to exceed to 200 bpm and can go into VF or pulseless VT. In VT the P waves cannot be identified and T waves are opposite in polarity to QRS. Some causes of VT include: drug toxicity, prolonged QT syndrome, myocarditis, underlying heart disease, and electrolytes disturbances.
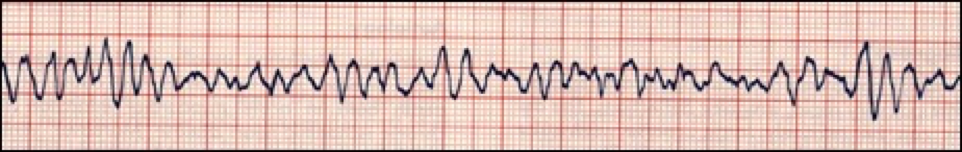
Torsades de Pointes/Polymorphic VTPolymorphic VT or Torsades de Pointes is when different areas in the ventricles fire fast, uncoordinated impulses. Ventricular rates range from 150-250 bpm and QRS complex vary in apprearance. Some causes of polymorphic VT or Torsades de pointes include: diarrhea, hypomagnesaemia, and hypokalemia.
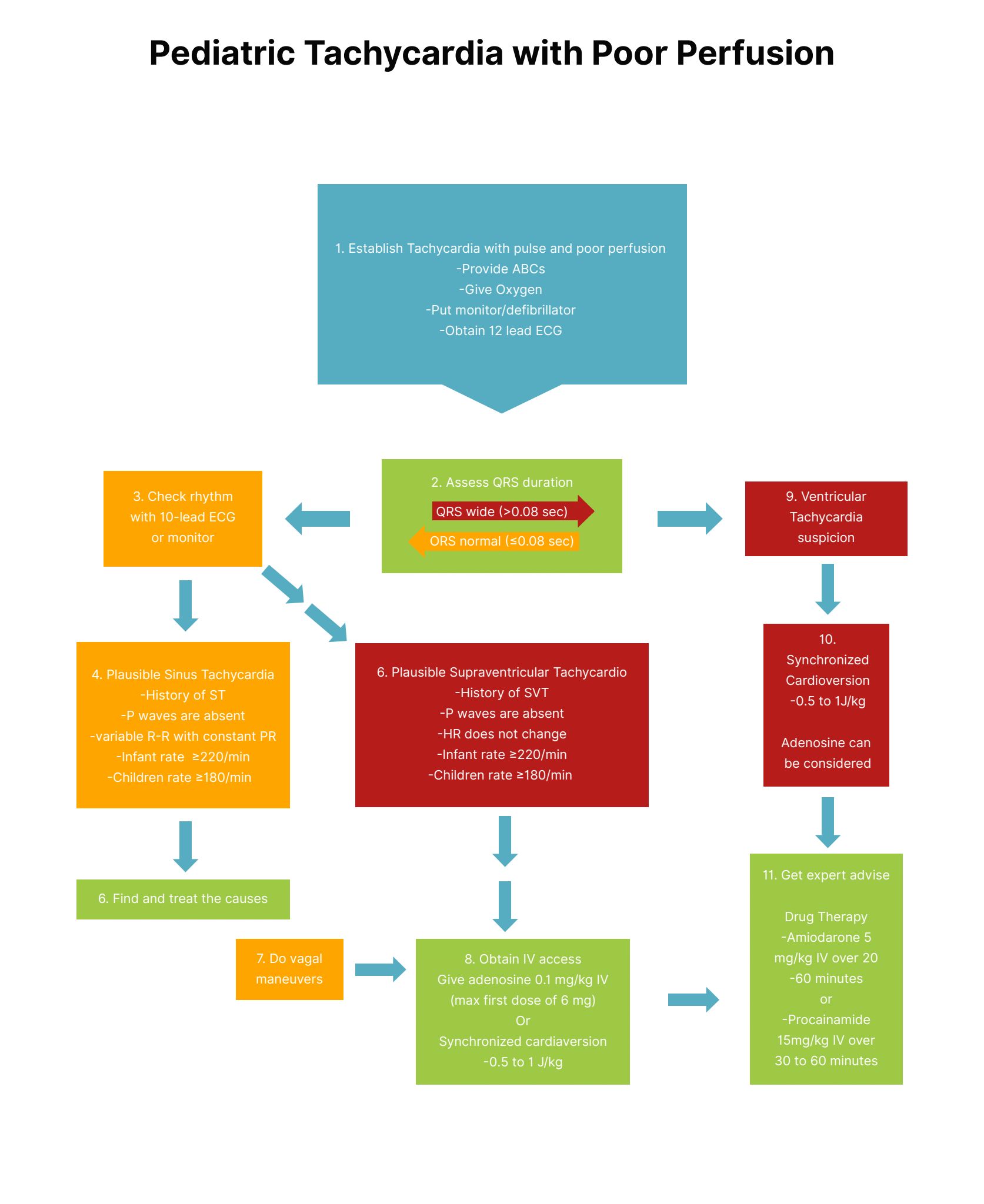
Management of TachyarrhytmiasUpon recognizing the child with tachycardia immediately activating the EMS and conducting the ABCs
The following algorithms show management of tachycardia with a pulse and adequate perfusion and one with poor perfusion for children.
|
|||||||||||||||||||||
Cardiac dysrhythmia or arrhythmias are caused by abnormalities in the electrical activity of the heart and can be classified as bradyarrhythmias, tachyarrhythmias or pulseless arrest. They are associated with an increased heart failure. Cardiac arrhythmias are accelerated, irregular or slow heart rates caused by abnormalities in the myocardium.
Bradyarrhythmias are the most common arrhythmias in children and usually presents with hypoxemia, hypotension and acidosis. Bradycardia is a heart rate which is slower than the normal for the age of the child; usually less than 60 bpm is indicative of bradycardia and immediate CPR should be initiated.
| Signs of Bradycardia |
|
|
|
|
| Symptoms of Bradycardia |
|
|
|
|
There are 5 examples of bradyarrthmias that are seen in children:
Sinus node arrest/sick sinus syndrome is associated with abnormal heart rhythms due to malfunction of the sinus node. These may include atrial, junctional and idioventricular escape rhythms.
Sinus bradycardia starts in the SA node with decreased rate (<60 beats/min). It develops due to decreased metabolic demand and may be caused by hypoxia, poisoning, hypoglycemia, or hypothyroidism.
First Degree AV Block
First degree AV block is when the PR interval is prolonged (> 0.20 seconds) and impulse from atria to ventricles through the AV node is delayed. There usually are no symptoms associated with first-degree AV block.
Second Degree AV Block Type I
2nd Degree AV block type I (Wenckebach-Mobitz I) is when the PR intervals are prolonged, R-R intervals are shortened and finally one beat drops. Symptoms may include dizziness, but usually not seen.
Second Degree AV Block Type II
2nd degree AV block Type II (Mobitz II) is when there is no change in the PR interval and then a beat will drop randomly. Symptoms may include irregular heart bear, presyncope or syncope.
Third Degree AV Block
3rd degree Av block is a complete heart block where the P wave and QRS complexes are not connected. Impulse conducted in the atrium does not progress to the ventricles. There is no communication between the atrium and the ventricles. Symptoms include fatigue, presyncope or syncope.
Proper management of bradyarrhythmia includes managing for heart rate and respiratory distress or failure. The following are steps in the treatment of bradycardia:
Upon recognizing the child is bradycardic immediately activating the EMS and conducting the ABCs
After one round of CPR give the following doses of medications:
Tachyarrhythmias are considered fast abnormal rhythms, which originate from the atria or ventricles. Tachycardia is a heart rate which is faster than the normal for the age of the child; and immediate CPR should be initiated.
| Signs of Tachycardia |
|
|
|
|
| Symptoms of Tachycardia |
|
|
|
|
The following are examples of tachycardia:
Atrial flutter is abnormal heart rhythm causing fast irregular heartbeat. Usually occurs in the atria of the heart and is uncommon in children. Some causes of atrial flutter include: hypertension, ischemia, cardiomyopathy, and abnormal heart valve.
Sinus tachycardia is when the rate of impulse from the SA node is elevated than normal for age. Heart rate <220 bpm in infants, <180 bpm in children, P wave is normal, PR interval is constant, and R-R interval is variable. Some causes of ST include: hypoxia, hypovolemia, fever, poison, metabolic stress, trauma, pain, anxiety, toxicity, and anemia.

Supraventricular Tachycardia (SVT) is a rapid heartbeat that starts right above the ventricles. SVT is the most common cause of tachyarrhythmia in infants causing cardiac issues. Heart rate >220 bpm in infants, >180bpm in children, p wave is abnormal; R-R interval is constant. Some causes of SVT include: AV nodal reentry, ectopic atrial focus, and accessory pathway entry.

Ventricular tachycardia (VT) starts in the ventricles and is uncommon in children, and the heart rate is regular and at least 120 bpm. VT with pulse can cause the heart rate to exceed to 200 bpm and can go into VF or pulseless VT. In VT the P waves cannot be identified and T waves are opposite in polarity to QRS. Some causes of VT include: drug toxicity, prolonged QT syndrome, myocarditis, underlying heart disease, and electrolytes disturbances.
Polymorphic VT or Torsades de Pointes is when different areas in the ventricles fire fast, uncoordinated impulses. Ventricular rates range from 150-250 bpm and QRS complex vary in apprearance. Some causes of polymorphic VT or Torsades de pointes include: diarrhea, hypomagnesaemia, and hypokalemia.
Upon recognizing the child with tachycardia immediately activating the EMS and conducting the ABCs
Evaluate the QRS complex as either normal or wide
If normal QRS:
If wide QRS:
The following algorithms show management of tachycardia with a pulse and adequate perfusion and one with poor perfusion for children.