|
Chapter 21 : Stable TachycardiaTachycardia is when the heart rate or rhythm is too fast (>100 beats/min). Conservative measures can be applied to stable tachycardia patients after deciding whether they have a narrow or wide QRS complex. Increase in heart rate causes less blood to be pumped through the systemic and pulmonary systems. Low blood flow will cause less oxygen to flow to the heart and brain and less oxygen to the heart can lead to Ischemia and MI. In stable tachycardia the patient is stable and no significant signs and symptoms are present. Stable Tachycardia Video:Stable Tachycardia Include:
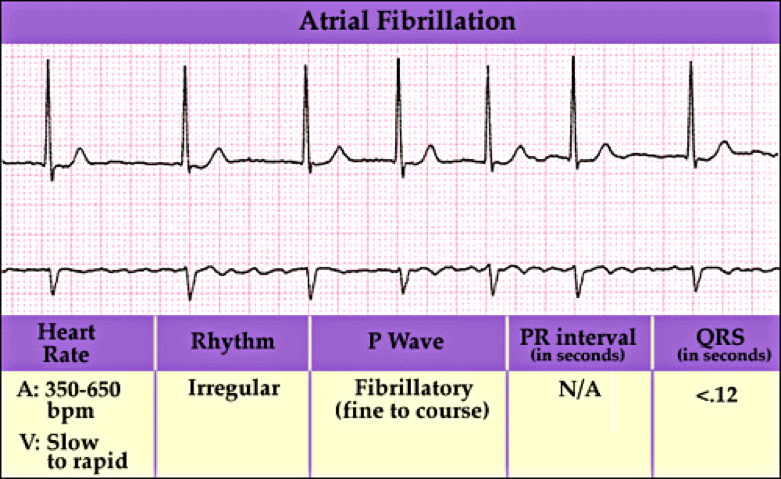
Atrial fibrillation is when the heart beats do not occur at the same intervals. It is known as the quivering of the muscles and involves both the atriums of the heart.
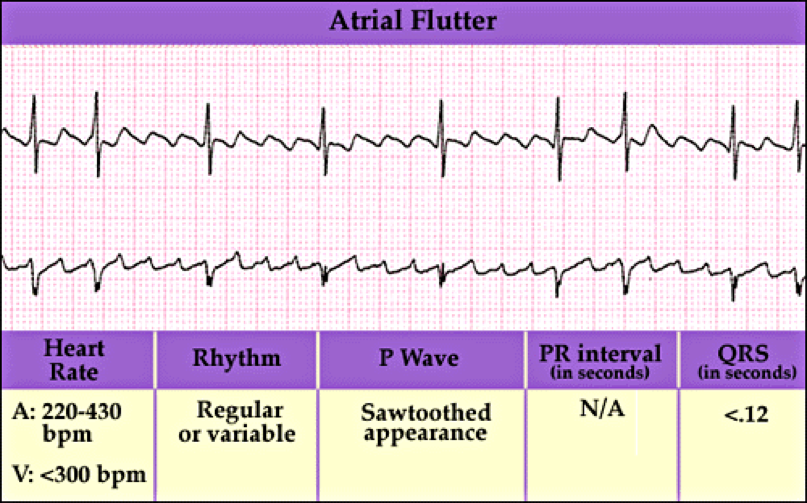
Atrial flutter is abnormal heart rhythm causing fast irregular heartbeat. Starts in the atrium and can lead to atrial fibrillation. Usually has a ‘saw-toothed’ appearance.
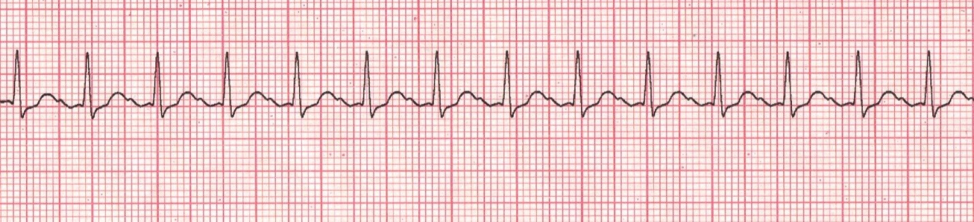
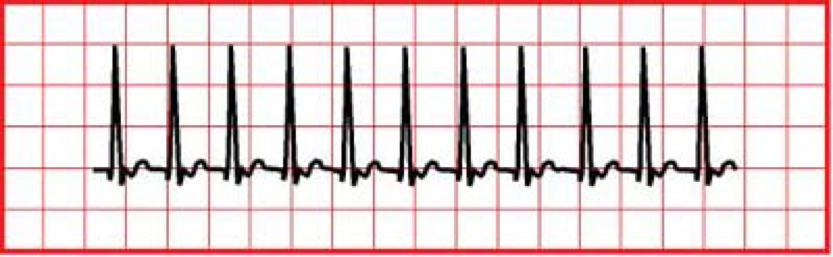
Sinus tachycardia is when the rate of impulse from the SA node is elevated.
AV nodal reentry is a heart rhythm that is seen due to the malfunctioning of the AV node. It is the most common type of SVT
Supraventricular Tachycardia (SVT) is a rapid and narrow heartbeat that starts in the atria or AV node.
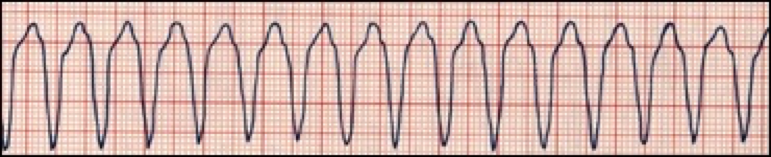
Monomorphic VT is heart rate of >150 bpm but QRS complexes look the same.
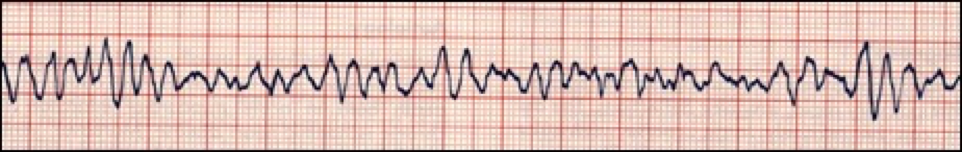
Polymorphic VT is when different areas in the ventricles fire fast, uncoordinated impulses.
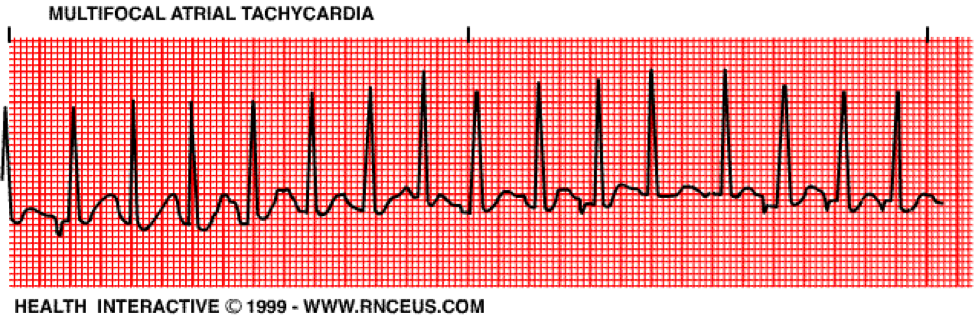
Multifocal Atrial Tachycardia is when the atrial pacemaker rhythm is deranged and causes the ventricular rate to be greater than 100 bpm. This rhythm causes the P waves to differ in size, shape and direction.
Scenario: You are the night nurse on duty and a 40 year old woman is complaining of palpitations. She mentions that she has a history of recurrent heart rates and she feels she’s having a heart attack. Stable Tachycardia Assessment:
Stable Tachycardia Interventions:
Stable Tachycardia Management:
The following is an algorithm showing management of stable tachycardia in detail.
If a patient shows stable tachycardia they will not present with hypotension, shock, ischemic chest pain, AMS or heart failure. In a case when the patient is stable and has regular rhythm, consider administering adenosine and attempting to do vagal maneuvers. Vagal maneuvers and administration of adenosine is the initial first line intervention for narrow complex stable tachycardias. These maneuvers initiate baroreceptors in the aortic arch and the internal carotid arteries, which then cause stimulation of the Vagus nerve which releases acetylcholine. The acetylcholine reduces AV node conduction and that eventually slows down the heart rate. Types of Vagal Maneuvers
If regular SVT is not fixed by adenosine or vagal maneuvers then the best option is to seek expert advice. Learning Outcomes:You have completed Chapter XVI. Now you should be able to:
|
Tachycardia is when the heart rate or rhythm is too fast (>100 beats/min). Conservative measures can be applied to stable tachycardia patients after deciding whether they have a narrow or wide QRS complex. Increase in heart rate causes less blood to be pumped through the systemic and pulmonary systems. Low blood flow will cause less oxygen to flow to the heart and brain and less oxygen to the heart can lead to Ischemia and MI. In stable tachycardia the patient is stable and no significant signs and symptoms are present.
Atrial fibrillation is when the heart beats do not occur at the same intervals. It is known as the quivering of the muscles and involves both the atriums of the heart.
Atrial flutter is abnormal heart rhythm causing fast irregular heartbeat. Starts in the atrium and can lead to atrial fibrillation. Usually has a ‘saw-toothed’ appearance.
Sinus tachycardia is when the rate of impulse from the SA node is elevated.
AV nodal reentry is a heart rhythm that is seen due to the malfunctioning of the AV node. It is the most common type of SVT
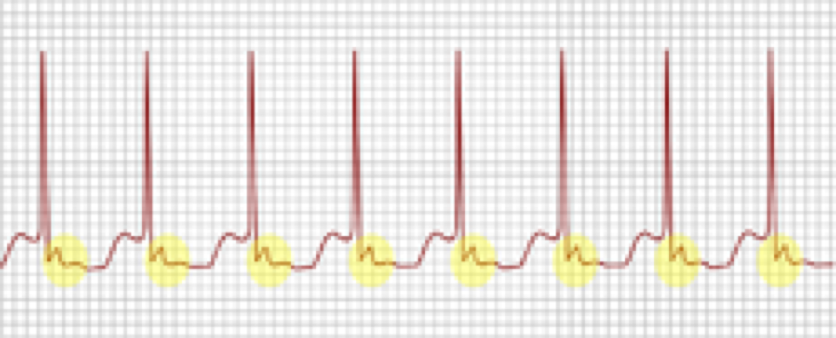
Supraventricular Tachycardia (SVT) is a rapid and narrow heartbeat that starts in the atria or AV node.
Monomorphic VT is heart rate of >150 bpm but QRS complexes look the same.
Polymorphic VT is when different areas in the ventricles fire fast, uncoordinated impulses.
Multifocal Atrial Tachycardia is when the atrial pacemaker rhythm is deranged and causes the ventricular rate to be greater than 100 bpm. This rhythm causes the P waves to differ in size, shape and direction.
Scenario: You are the night nurse on duty and a 40 year old woman is complaining of palpitations. She mentions that she has a history of recurrent heart rates and she feels she’s having a heart attack.
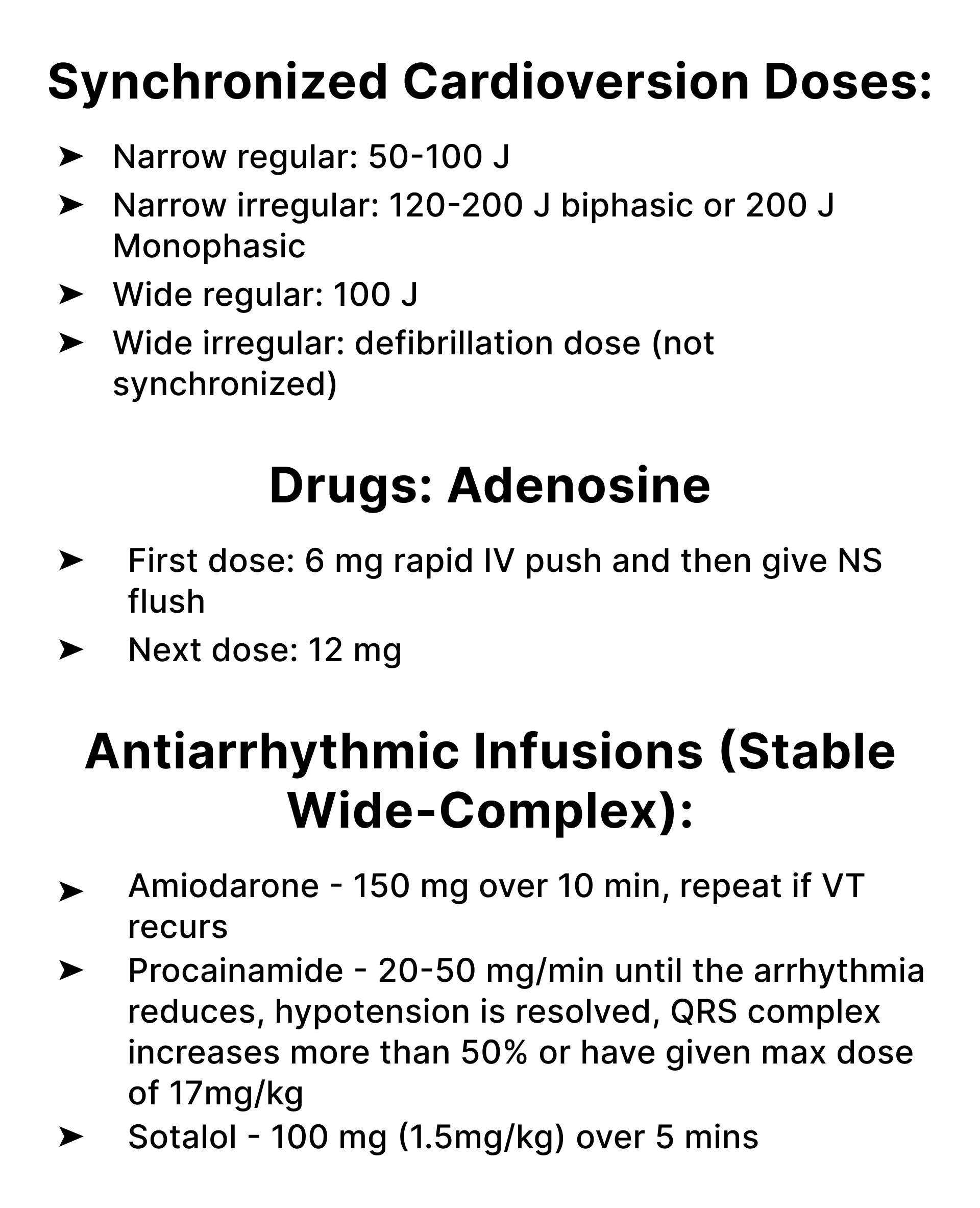
If persistent tachyarrhythmia initiate synchronized cadioversion
The following is an algorithm showing management of stable tachycardia in detail.
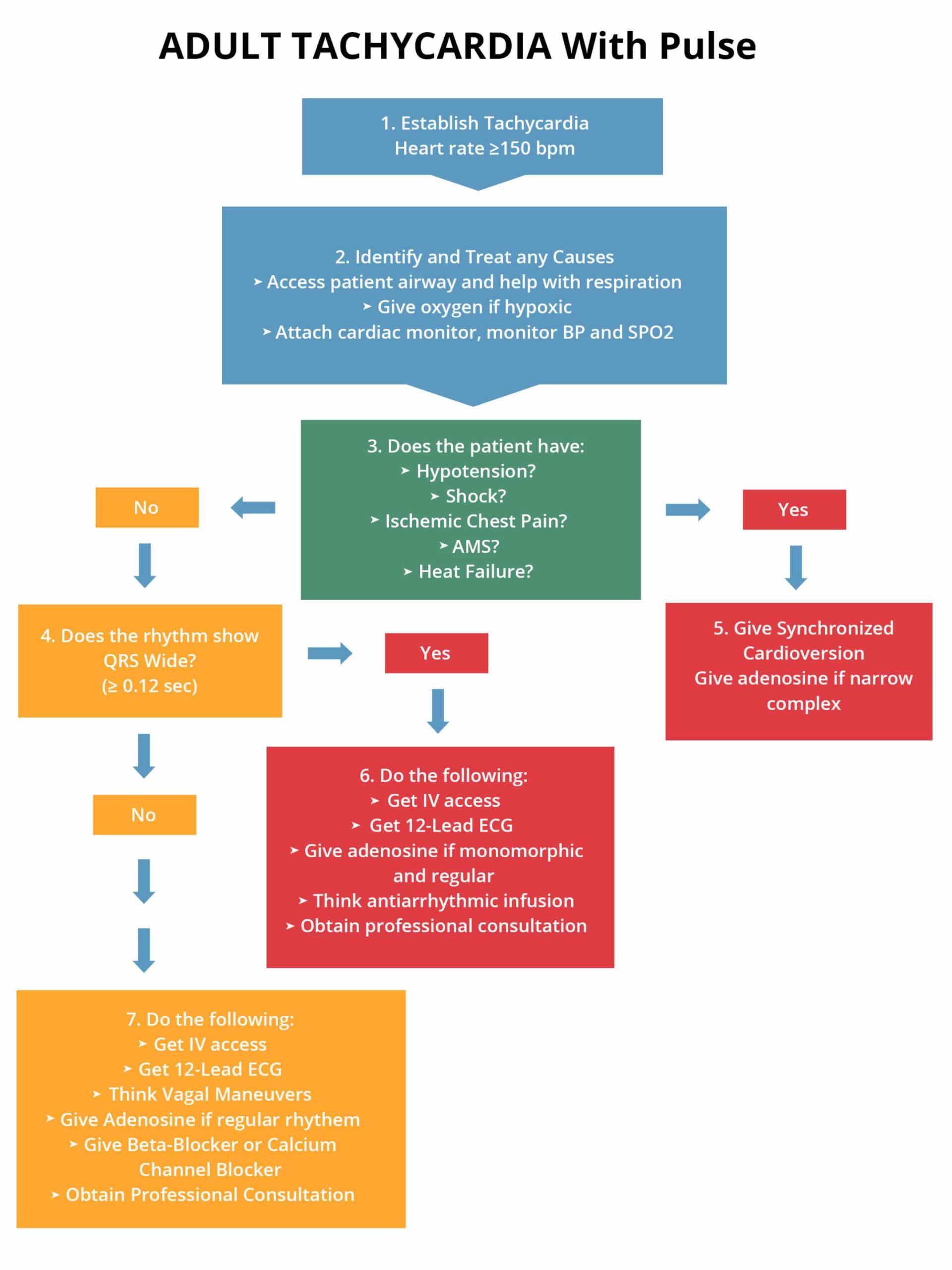
If a patient shows stable tachycardia they will not present with hypotension, shock, ischemic chest pain, AMS or heart failure. In a case when the patient is stable and has regular rhythm, consider administering adenosine and attempting to do vagal maneuvers.
Vagal maneuvers and administration of adenosine is the initial first line intervention for narrow complex stable tachycardias. These maneuvers initiate baroreceptors in the aortic arch and the internal carotid arteries, which then cause stimulation of the Vagus nerve which releases acetylcholine. The acetylcholine reduces AV node conduction and that eventually slows down the heart rate.
If regular SVT is not fixed by adenosine or vagal maneuvers then the best option is to seek expert advice.
You have completed Chapter XVI. Now you should be able to: