|
Chapter 17 : AsystoleAsystole or ‘flatline’ is associated with no cardiac electrical activity, no contraction of the heart muscle and no cardiac output. Flatline is when there is a straight line on the monitor, but asystole is when there is an actual absence of electrical activity. The first step is to ensure that it is an actual asystole by making sure of the following:
Asystole ACLS Training Video:
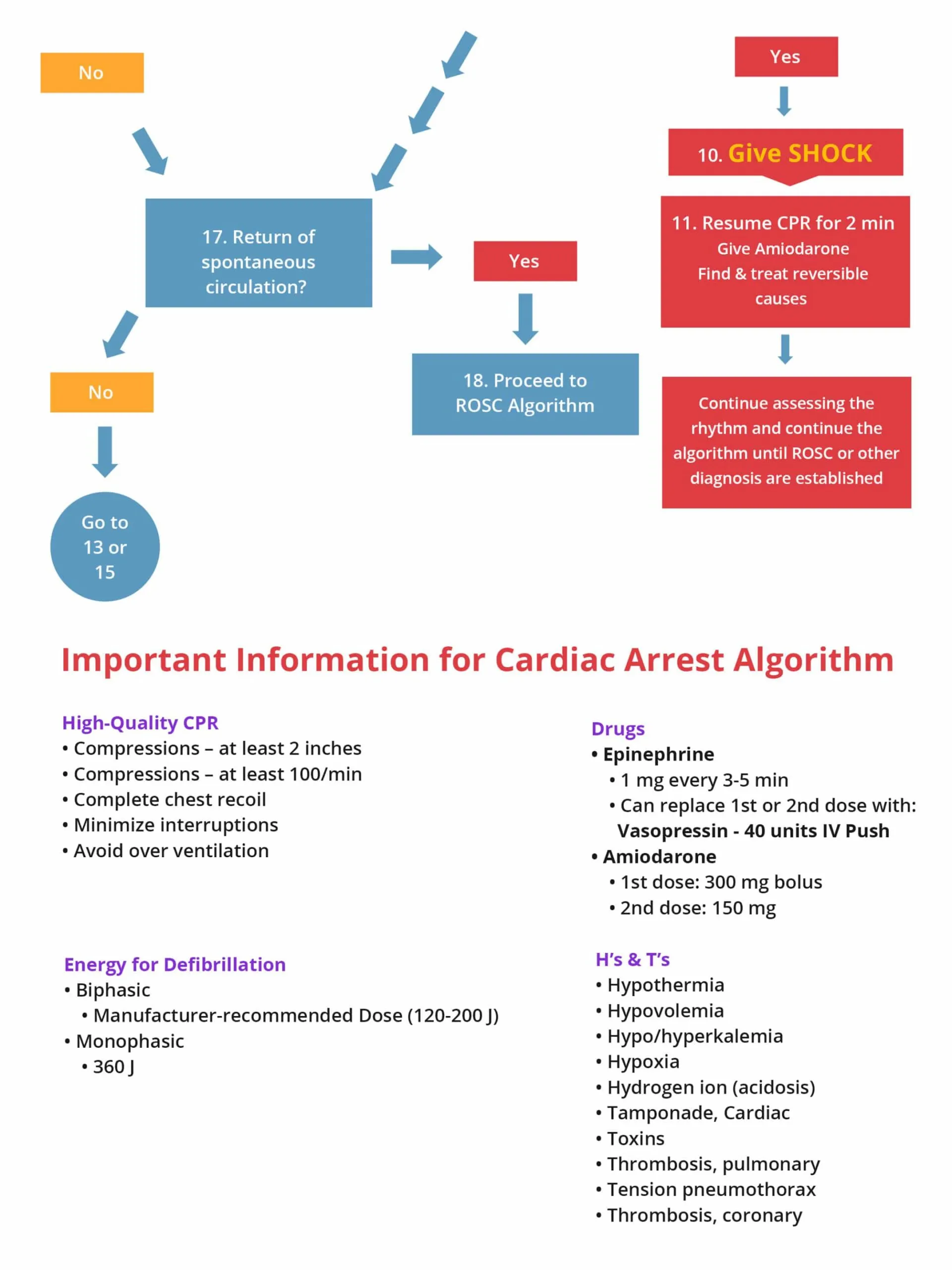
Asystole can be caused by many factors and are represented as H’s and T’s:
Scenario: You are a paramedic and arrive on the scene. A man is lying on the floor unconscious and the neighbor tells you that she saw the man collapse as he was unlocking his front door. Assessment:
Interventions:
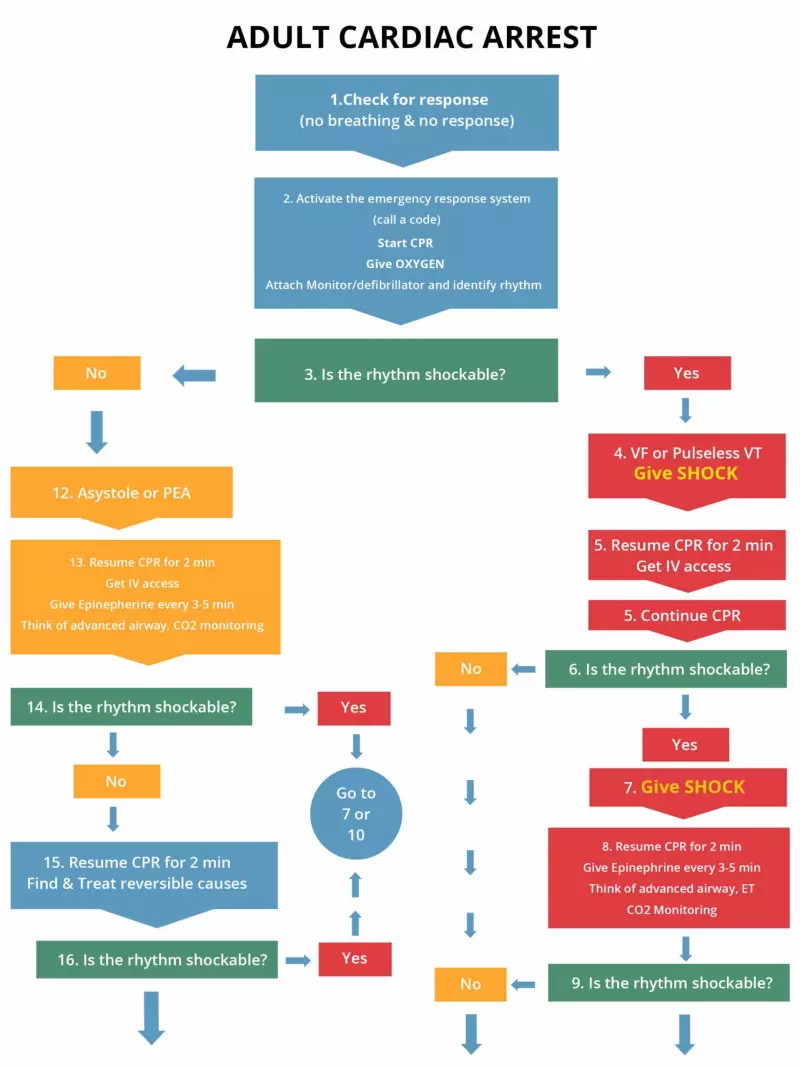
Management: AT the hospital initiate the cardiac arrest algorithm on the right if the patient still has no pulse and does not respond to BLS. Get a code team in place.
The following is an algorithm shows management of cardiac arrest due to a flat line situation or asystole/PEA (left side of chart)
Note: When conducting the BLS and ACLS survey on a patient with asystole, there may be times when you should hold resuscitative efforts; those include:
Learning Outcomes:You have completed Chapter XII. Now you should be able to:
|
||||||||||||
Asystole or ‘flatline’ is associated with no cardiac electrical activity, no contraction of the heart muscle and no cardiac output. Flatline is when there is a straight line on the monitor, but asystole is when there is an actual absence of electrical activity. The first step is to ensure that it is an actual asystole by making sure of the following:
| H’s | T’s |
| Hypovolemia – Decreased blood volume | Tension pneumothorax – air in the pleural space around the lung (lung collapses) |
| Hypoxia- decreased partial pressure of oxygen in blood | Tamponade – compression of the heart produced by excess fluid surrounding the heart |
| Hydrogen ion (acidosis) – Increase in the concentration of H ions in blood | Toxins – poisonous substances |
| Hyper-/hypokalemia –abnormally high or low potassium concentration in the blood | Thromobosis (pulmonary) – formation of a blood clot which blocks a blood vessel in lungs |
| Hypothermia – body temperature less than 30 degrees C (86 degrees F) | Thrombosis (coronary) –formation of a blood clot which blocks a blood vessel in heart |
Scenario: You are a paramedic and arrive on the scene. A man is lying on the floor unconscious and the neighbor tells you that she saw the man collapse as he was unlocking his front door.
Assessment:
Interventions:
Management: AT the hospital initiate the cardiac arrest algorithm on the right if the patient still has no pulse and does not respond to BLS. Get a code team in place.
Once IV/IO access is obtained give the following drugs:
The following is an algorithm shows management of cardiac arrest due to a flat line situation or asystole/PEA (left side of chart)
Note: When conducting the BLS and ACLS survey on a patient with asystole, there may be times when you should hold resuscitative efforts; those include:
You have completed Chapter XII. Now you should be able to: