Postresusciation management occurs once the child’s health is under proper control and return of spontaneous circulation is achieved. The postresusciation method assesses the following organ system optimizes ventilation and circulation to ensure proper treatment techniques are applied for adequate management and recovery of the child.
The organ systems in the postresusciation methods are as follows:
- Cardiovascular
- Gastrointestinal
- Hematologic
- Neurologic
- Renal
- Respiratory
- Shock
PALS Certification By American HealthCare Academy Videos:
Cardiovascular
| Monitor |
- Heart rate and rhythm
- Blood pressure
- Spo2
- Urine output
|
| Monitor |
- Heart rate and rhythm
- Blood pressure
- Spo2
- Urine output
|
| Physical Examination |
- Quality of central and peripheral pulses, HR, temperature and color
- Monitor end-organ function
|
| Lab Test |
- Arterial blood gas
- Hemoglobin and hematocrit
- Serum glucose, electrolytes, BUN/creatinine, Calcium
- Lactate and central venous oxygen saturation
|
| Non Lab Tests |
- Chest x-ray to check ET tube insertion, heart size, pulmonary edema, etc
- 12-lead ECG
- Echocardiogram
|
| Intravascular Volume |
- Get vascular access
- Give fluid boluses of 10 to 20 mL/kg of isotonic crystalloid over 5 to 20 minutes
- Blood administration
- Maintain fluid
|
| Blood Pressure |
- Treat hypotension with vasoactive drugs
- Treat arrhythmia if hypotension is due to that
- Give vasopressor for vasodilation induced hypotension
|
| Tissue Oxygenation |
- Give supplementary oxygen
- Support perfusion
- Maintain hemoglobin concentration
- Targeted temperature management to achieve ROSC normal paCO2 35-45 mmHg
|
| Metabolic Demand |
- Pain control with morphine or fentanyl
- Agitation control with sedation
- Fever maintenance with antipyretics
- ET tube and ventilation to control breathing
|
| Arrhythmias |
- Tachyarrhythmias and bradyarrhythmias with medicine and cardioversion
- Expert consultation
|
| Postarrest Myocardial Dysfunction |
- Postarrest myocardial dysfunction for 4 to 24 hours after ROSC
- Vasoactive agents to fix hemodynamic functions
- Maintain blood pressure and perfusion
|
Gastrointestinal
| Monitor |
- Monitor type and quality of nasogastic tube drainage
|
| Physical Exam |
- Abdominal examination and check for bowel sounds, girth and tightness
|
| Lab Tests |
- Liver function by ALT/AST, albumin, PT/PTT, bilirubin, glucose, ammonia, etc tests
- Pancreatic function by amylase/lipase tests
|
| Non Lab Tests |
- Ultrasound to check liver, gall bladder, pancreas and bladder
- Abdominal CT scan to check for trauma
|
| Gastric Distention |
- Put in orogastric or NG gupe to aspirate stomach air and contents
- Inseart NG feeding tube
|
| Ileus |
- Put in OG or NG to aspirate gastric fluids and contents
- Maintain electrolyte and fluid balance
|
| Hepatic Failure |
- Administer glucose
- Correct clotting factor and use fresh frozen plasma for bleeding
|
Hematologic
| Physical Examination |
- Find cause of external or internal hemorrhage
- Check skin for pallor, petechiae or bruising
|
| Lab Tests |
- Hemoglobin and hematocrit
- Platelet count
- Prothrombin time,PTT, INR, fibrinogen, and D-dimer
|
Neurologic
| Monitor |
- Check and control temperature
|
| Physical Examination |
- Conduct neurologic assessment by checking pupil response, gag reflex, corneal reflex, etc
- Check for cerebral herniation
- Identify seizures
- Check normal and abnormal movements and neurologic findings
|
| Lab Tests |
- Check glucose levels
- Check serum electrolyes and calcium concentration
- Check for overdosage and poisons
- Conduct cerebral spinal fluid studies
|
| Non Lab Tests |
- CT scan
- EEG for convusions or epileptic seizures
|
| Brain Perfusion |
- Support cardiac output and oxygen
- Avoid hyperventilllation
|
| Blood Glucose |
- Treat hypoglycemia
- Check glucose concentration
- Treat hyperglycemia
|
| Temperature Control |
- Control hypothermia and hyperthermia. Emphasis on targeted temperature management to achieve ROSC (Return of Spontaneous Circulation).
|
| Increased ICP |
- Head in midline
- Ventilate
- Give steroids for inflammation or CNS tumor
- Use mannitol or saline for herniation
|
| Seizures |
- Treat seizures with benzodiazepine, fosphenytoin/phenytoin or barbiturate
- Correct metabolic causes
- Check for toxins or other diseases
|
Renal
| Monitor |
- Check for decreased urine output (<1 mL/kg per hour in infants and children)
- Check for increased urine output due to glucosuria or DI
|
| Physical Examination |
- Check abdomen for distended bladder or tight abdomen
- Check for hypovolemia
- Check urinary catheter placement
|
| Lab Tests |
- Check renal function by BUN/creatining and serum electrolytes
- Get urinalysis
- Assess metabolic state by ABG, glucose, anion gap and lactate concentration
|
| Renal Function |
- Resore intravsasuclar volume and systemic perfusion with vasoactive drugs
- Administer loop diuretics to those with volume overload and CHF
- Put KCL to IV fluids if renal function is poor or no urine output
|
| Acid-base Balance |
- Fix lactic acidosis with vasoactive agents and improving tissue perfusion
- Fix non-anion gap with sodium bicarbonate
|
Respiratory
| Monitor |
- Spo2 and heart rate by pulse oximetry
- Heart rate and rhythm
- Exhaled CO2 by colorimetric device
- Check intubation
|
| Physical Examination |
- Check chest rise and auscultation of abdomen and breath sounds
- Check for tachypnea, agitiation, difficulty in breathing, cyanosis, and poor gas exchange
|
| Lab Tests |
- Get arterial blood gas (ABG)
|
| Non Lab Tests |
- Get chest x-ray for check for any pulmonary problems and placement of ET tube
|
| Oxygenation |
- Give oxygen and check for Spo2 ≥ 94-99%
- If less than 94% give additional ventilation support
|
| Respiratory Failure |
- ET intubation
- Gastric tube insertion to eliminate gastric contents
|
| Analgesia and Sedation |
- Control pain with fentanyl or morphine
- Sedation with lorazepam or midazolam
|
| Neuromuscular Blockade |
- For intubated children give becuronium and pancuronium or other neuromuscular blocking agents
|
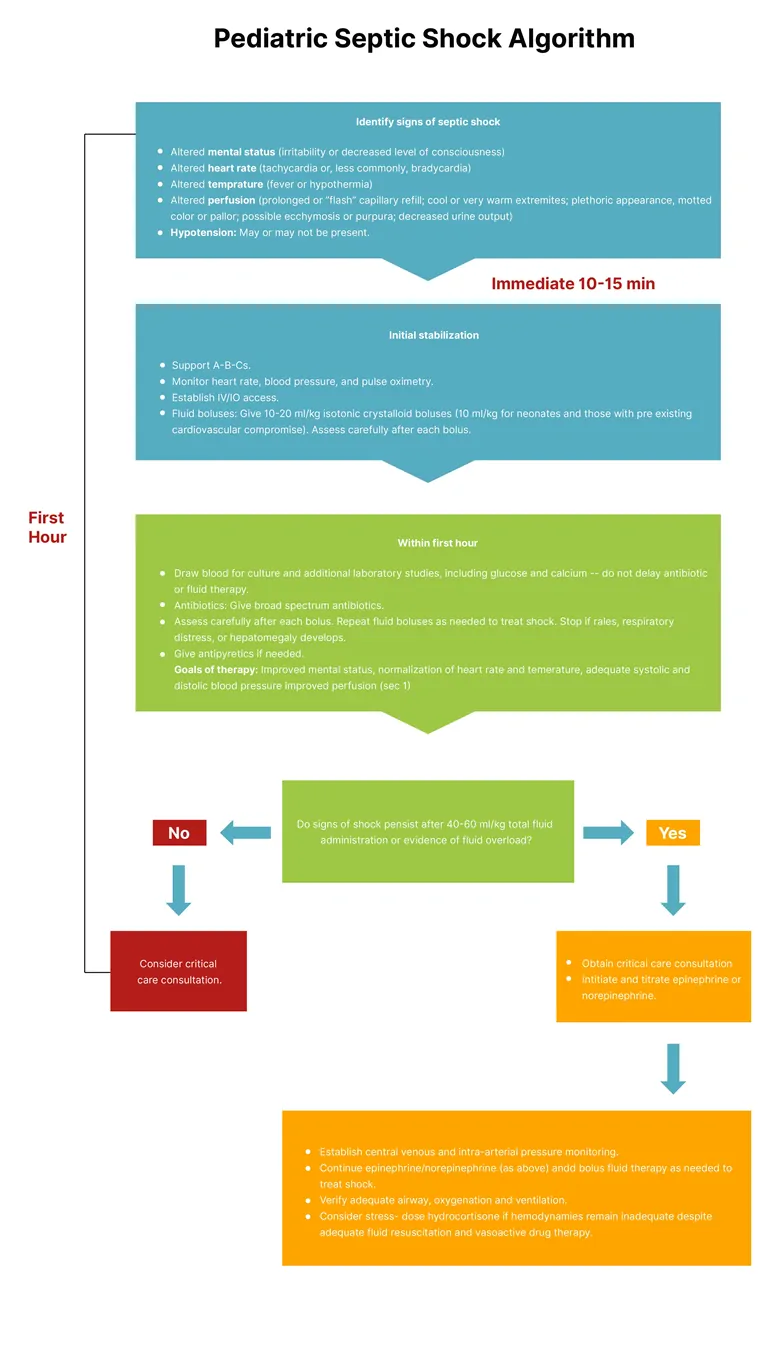
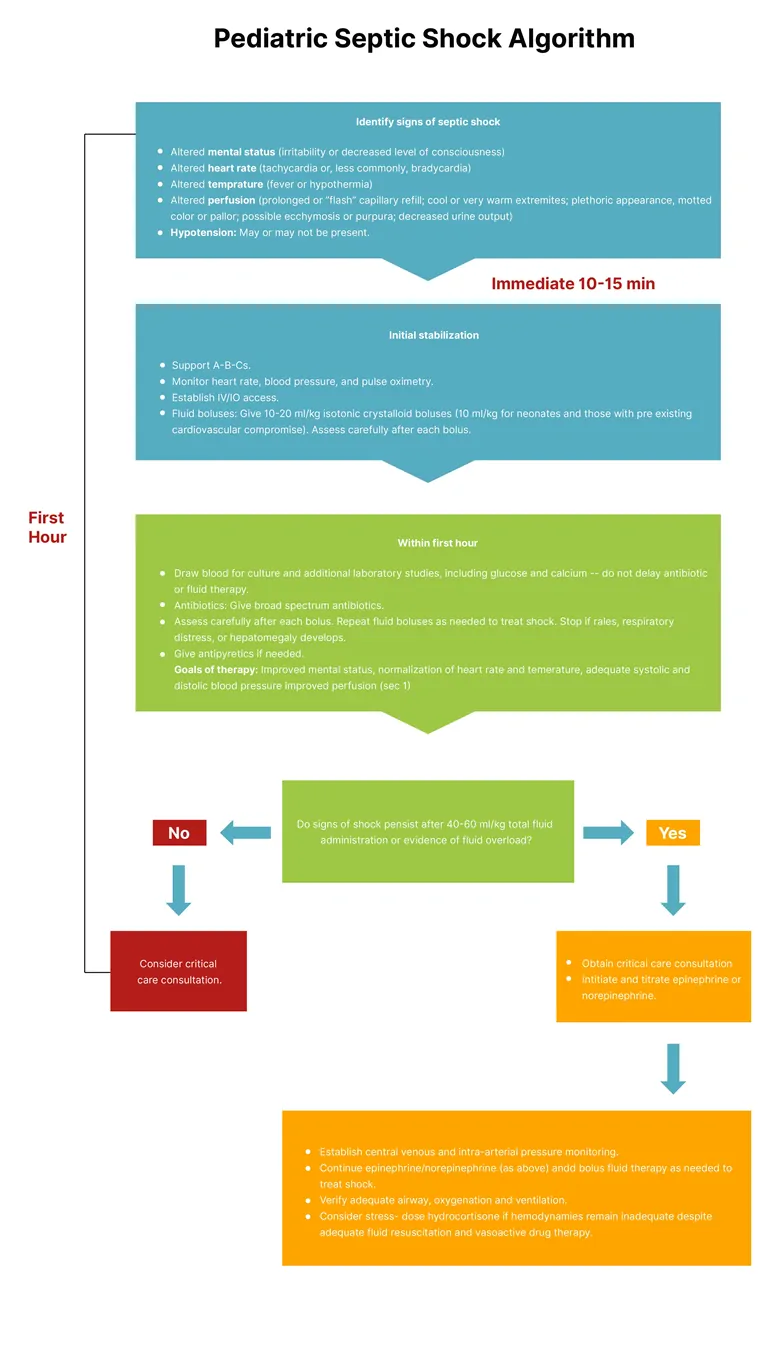
Shock
The following algorithm displays PALS postresusciative methods for shock: