Thank you for signing up!
Check your email, the 10% OFF coupon is in your inbox.

*This course now follows updated ECC guidelines for Basic Life Support (CPR) in relation to the resuscitation of, suspected or confirmed, COVID-19 patients. Look for these interim updates throughout the course.
Sudden cardiac arrest (SCA) is a leading cause of death among adults in the United States. Cardiopulmonary resuscitation (CPR) dramatically increases the chance of survival for a victim suffering from SCA. Hence, an online CPR certification is imperative to save lives. Don’t be a bystander anymore and save a life. Learn this lifesaving skill today.
CPR is a combination of chest compressions and breaths, and provides critical blood flow and oxygen to the heart and brain.
If CPR is started within three to five (3-5) minutes of collapse, it increases a victim’s chance of survival and reduces the chance of permanent damage.
This course follows the most recent and updated ECC guidelines, and has been designed to help you acquire the skills you will need to effectively respond in an emergency situation.
It is important to always check the scene and ensure your safety first. Remember to stay alert so you are able to identify and assist in an emergency.
2020 Interim Guidance for suspected or confirmed COVID-19 patients: Put on PPE immediately & limit the personnel around you after you verify that the scene is safe.
It is critical to understand that dialing 9-1-1 is one of the most important steps you can take to save another’s life.
While helping the victim, protect yourself from transmission of possible diseases.

PPE includes: Gloves, Goggles (eye protection) Gown, Lab Coat or Apron, Shoe Covers, Face Shields / Masks, and Cap
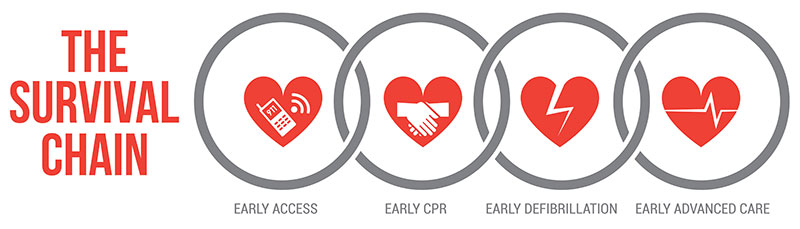
If you suspect that a victim has suffered a spinal or neck injury, do not move or shake the victim.When preparing to perform CPR, keep in mind ECC’s Chain of Survival. These are the five crucial steps that should be performed in an emergency:
ECC and AHA 2010 updates changed the CPR sequence from A-B-C to C-A-B. Often in the A-B-C method chest compressions were delayed. With the new Compressions – Airway – Breathing method a victim receives compressions faster, providing quicker critical blood flow to the vital organs.
The sequence of steps for conducting CPR using the C-A-B method (detailed further in following chapters)
“C” for Compressions
“A” for Airway
“B” for Breathing
2020 Interim Guidance for suspected or confirmed COVID-19 patients:
In these times when everyone is being affected by the Coronavirus disease (COVID-19), many lay responders/community rescuers are unlikely to have access to adequate PPE. They are also at an increased risk of exposure to COVID-19 during CPR, which might make individuals hesitant to act in times of cardiac emergencies.
However, lay rescuers of family members are likely to have already been exposed to COVID-19. Below are the primary interim changes to CPR during COVID-19 times.
PPE should be put on before conducting CPR.
For Adults:
For Children:
Per the 2015 updates, you should deliver at least 100 to 120 chest compressions per minute (previous rate was 100 compressions / minute). Recent science indicates that more compressions lead to a higher survival rate. This new update sets an upper limit for the chest compression rate, as excessive compressions and depth can adversely affect a patient’s outcome.
The Hands-Only CPR method is recommended for use on teens or adults that you witness suddenly collapse. This is CPR without the rescue breaths.
You would need to:
*The Good Samaritan Law is intended to reduce bystanders’ hesitation to assist in an emergency.
Before beginning CPR, follow these initial steps:
Check to see if the patient is breathing. Tap and shout, “Are you okay?” to see if victim is responsive. If unresponsive, continue with steps below.
Check the victim’s pulse Don’t take more than 10 seconds to check for the pulse. Begin CPR if you cannot locate or are unsure of a pulse.
** Note: [2020 Interim Guidance] During COVID-19, many lay responders are unlikely to have access to adequate PPE. Use a face mask or cloth to cover your, and the victim’s, mouth and nose to prevent transmission.
*Note: For CPR emergencies, an adult is anyone who is going through or gone through puberty.
Ensure that the victim is lying on his back on a firm, flat surface
Form the correct hand position for chest compressions:
After every 30 compressions, open the airway and give two rescue breaths. If you can give breaths, you will help the victim even more.
To give breaths you must first open the airway and ensure there are no obstructions. The tongue is the most common obstruction. If you see any foreign object and it can be removed easily, remove it.
Perform the head-tilt chin-lift motion: Tilt the head and pinch the nose with the same hand. With the other hand lift the chin – this will open up the airway.

Hold open the airway, pinch the nose, and blow air into the mouth. Be sure to place your mouth tightly over the victim’s mouth; use a barrier if available. Give 2 breaths that last one (1) second each. Ensure that the chest rises and falls between each breath.
If the breaths you give do not go in, continue to give chest compressions following the same 30:2 ratio until the breaths go in. Do not interrupt compressions for more than 10 seconds.
Continue to give sets of 30 chest compressions and 2 rescue breaths, with at least 100 to 120 compressions per minute until an AED or EMS arrives, or the person starts to breathe (shows signs of life).
If a person begins to breathe, roll him/her to their side in a recovery position until EMS arrives. When in recovery position, vomit and other fluids will drain from the mouth. While moving the person take special care of the neck, head and back.
** Note: [2020 Interim Guidance] Many lay responders may be hesitant to provide rescue breaths because of fear of transmission. Responders should at least perform hands-only CPR.
Now that you know the details of following the C-A-B method and performing Compressions, Opening the Airway, and Giving Breaths – let’s put the Adult CPR method together!
When a second rescuer is available to help, the duties are split amongst the two rescuers. The specific responsibilities of each in 2 rescuer infant CPR as well as adult CPR are listed below:
Rescuer 1 will begin to perform high quality chest compressions (at victim’s side).
This is a device which consists of a bag attached to a face mask and is readily available in a hospital setting. Using a bag valve mask is recommended for 2-rescuer CPR. It’s important to understand that the use of a bag-mask is difficult, and requires considerable practice before it can be done on a patient.
First, you must select a mask that will effectively cover the mouth and nose of a patient to create a tight seal. The patient’s face should be pulled up into the mask for best results (be sure not to crush the mask into the face). Then attach the mask to the bag device, which should be attached to high flow oxygen (15L per minute). The bag should be fully inflated.
Then perform the head-tilt chin-lift motion to open the airway, and give 2 breaths (1 second each). Be sure to watch for the rise and fall of the chest between breaths. If the patient’s chest does not rise and fall between each breath: check for obstructions, ensure that there is a tight seal to the face and that the airway is open.
Usually a child’s heart stops because of a breathing emergency. For this reason, giving breaths with compressions is very important for children.
When responding to a child in a CPR emergency follow the same steps for compressions, airway and breathing as detailed for adults. Listed below are the EXCEPTIONS for child CPR.

Usually an infant’s heart stops because of a breathing emergency. For this reason, giving breaths with compressions is very important for infants.
The process for responding to an infant is the same as responding to a child except for the following:


An Automated External Defibrillator (AED) machine shocks the heart and enables it to restart with a normal rhythm. The AED device will instruct you step-by-step, and will tell you to push a button if it determines that a shock is required.
A diagram will show you where to place the pads and when to restart compressions. If a second rescuer is present, he / she can help to attach AED pads while the first rescuer continues to perform CPR.
Child AED Usage: AED will instruct you to use child pads or a child key / switch.
*Remember if an AED is not present, start CPR immediately!
If an adult or child is choking, they may use the universal choking sign. This is when one holds the neck with one or both hands.
If you think that there is a conscious choking infant who cannot cough, cry or breathe, you will need to give 5 back blows and 5 chest thrusts. Follow these steps:

A breathing emergency (considered to be a medical emergency) is any respiratory problem that can threaten a person’s life. It can range from not being able to take a breath to not being able to breathe at all.
There are many different causes that can lead to a breathing emergency. Some of these include:
Asthma is the third highest cause of hospitalization amongst those under the age of 15. Many people that have this medical condition are aware of it and carry an inhaler for use in an emergency.
Asthma attacks can be triggered by many things, such as:

Ask the person if he/she has prescribed medication. Get the medicine for the person if he/she cannot access it.
A choking emergency (considered to be a medical emergency) is when an obstruction (object or food) blocks the airway and prevents air from getting to the lungs. The person is not able to breathe normally or cough. This section covers adult and child choking emergencies.
The relationship between the brain and its central nervous system is very interrelated with the functioning of each and every other part of the body. The nervous system controls: the five senses (sight, smell, taste, hearing, touch), the ability to think and reason, voluntary and involuntary functions, and regulates blood flow and blood pressure.
For this reason, head and spinal injuries may have a very significant effect on another part of the body. Prompt and timely First Aid given to nervous system emergencies is very crucial.
There are many different causes, mild or severe, that can lead to a nervous system emergency. Some of these conditions and injuries include:
A heart attack develops when blood flow is blocked and a segment of your heart muscle / tissue dies or is damaged.
Most commonly you can tell if someone is having a heart attack if they complain of chest pain. They may also experience uncomfortable pressure, nausea, shortness of breath, and/or discomfort in the arms, back, neck, jaw and abdomen.

A seizure is a sudden attack, which involves abnormal electrical activity in the brain. A person may experience mild shakes or more severe convulsions (rapid and uncontrollable shaking). Most seizures will stop within a few minutes of onset.
Seizures can be caused by head injuries, poisons, missed medications, low blood sugar or a medical condition called epilepsy.
A stroke usually occurs very suddenly when there is a problem with the blood supply to the brain. The supply gets blocked or a blood vessel within the brain ruptures.
Some specific signs and symptoms include: sudden and severe headache, dizziness, loss of consciousness or balance, slurred speech, drooling, inability to understand words, weakness, and/or paralysis on one side of the body.
The spinal cord primarily transmits signals between the brain and the rest of the body, and controls reflexes. Injuries to the spine can cause a person to lose the ability to move parts of the body.
A person may have a spinal or head injury if he/she was struck in the head/spine, fell, was assaulted, experienced a sports injury, or was in a car / motor vehicle accident (without a helmet).
The person may suddenly get sleepy, experience nausea, vomit, get a headache, have trouble walking and talking or not respond all together.
If person is experiencing:
When a person has an allergy, he or she experiences an immune response to a substance that is usually not harmful. An allergy emergency may occur if a person is exposed to this allergen. An allergic reaction may become severe if not treated in a timely manner.
People may be allergic to a variety of different things such as:
This is a severe, life-threatening allergic reaction. It occurs suddenly, and within seconds or minutes after contact with the allergen. A reaction of troubled breathing can cause obstructions in the airway and even lead to shock. Anaphylaxis requires immediate medical treatment, including the epinephrine injection and a trip to the hospital.
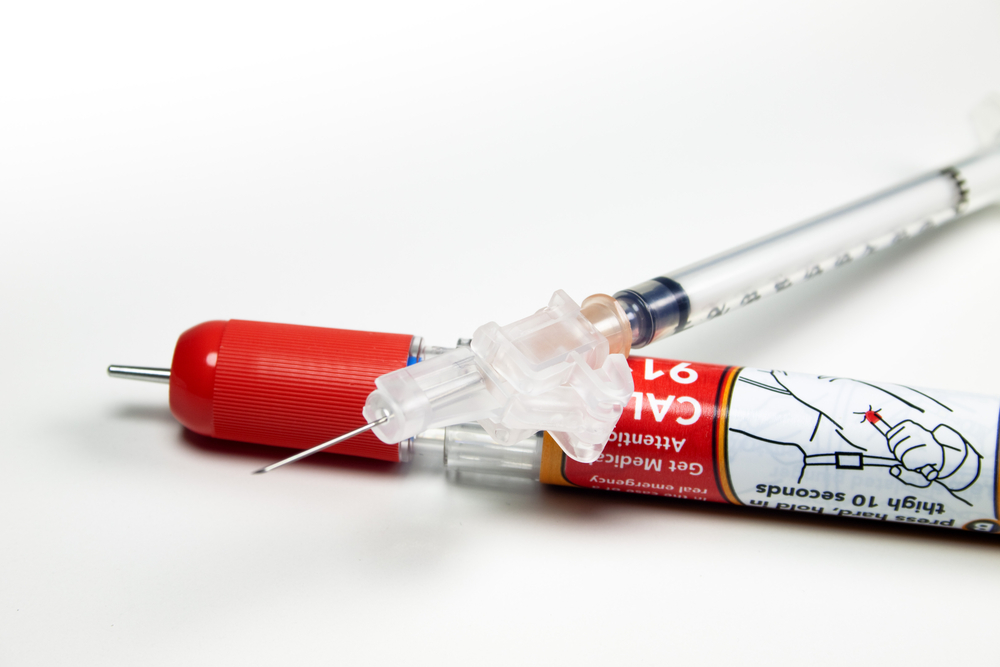
Accidents from bites and stings can happen at home, work or even while you are traveling. It’s important to understand the various types of bites and stings and what First Aid care should be provided. If one experiences an allergic reaction to the bite / sting, First Aid may involve the use of an epinephrine pen (Chapter 7).
A bite that punctures the skin can cause bleeding and lead to an infection. Bites that do not break the skin may require minor First Aid. It’s important to understand that the reaction to a punctured bite will vary depending on the germs that were in the biter’s mouth / saliva. If you notice that an animal is acting strangely, be sure to keep your distance. Some animals may carry rabies and require immediate medical attention, i.e., dog, cat, skunk, bat, raccoon or other wild animals.

Poisonous snakes release venom when they bite. You should always assume that a snake is poisonous if you are not able to tell from the bite mark. Symptoms of a poisonous snakebite can include: pain, swelling near the bite area, nausea, vomiting and weakness.
Unless a person is allergic to the source of the sting, a person may experience a minor reaction. Stings usually lead to itching, swelling and minor pain. Remember some stings may be more dangerous, if the source is poisonous (i.e., scorpion, poisonous spider). In these instances a person will experience more severe symptoms such as: fever, severe pain, seizures, vomiting, breathing problems and may even stop responding.
If person is experiencing:
Wounds are an injury of the soft tissue (tissue in the body that is not bone). Wounds are generally classified as either a closed or open wound.

A closed wound is a wound on the skin’s surface that does not break the skin. A common closed wound is a bruise, which develops when the body is bumped or hit. A more serious closed wound may be caused by a violent force hitting the body. The person can severely damage tissues, blood vessels and muscles, leading to heavier internal bleeding.
An open wound causes a break in the skin. The wound can range from something minor like a scrape to a deeper, puncture of the skin. A minor open wound includes small cuts, scrapes and abrasions. Immediate medical attention may be required for major open wounds that are heavily bleeding (i.e., amputation).
If person is experiencing:
This emergency occurs when a muscle, bone or joint moves in a direction that it is not supposed to go. This movement can lead to broken bones, sprains, fractures and other injuries.
A fracture is a complete break, a chip or a crack in the bone. An open fracture involves an open wound, and is when a bone end tears through the skin. An open fracture is more dangerous and severe. However, a closed fracture is more common.

A dislocation is the movement of a bone at a joint from its normal position. When the bone is moved out of place, the joint no longer functions. Usually, dislocations happen at the shoulder, elbow, wrist, jaw and hip.
A sprain is the tearing of the ligaments at a joint. Sprains mostly occur at the ankle, knee, wrist and fingers. A strain is the stretching and tearing of a muscle. They usually occur in the neck, back, thigh, or the back of the lower leg.
Use RICE method when dealing with a sprain or strain:

Rest:
Do not move or straighten the injury.
Immobilize:
Try to stabilize the person in the position he/she was found. Splint or sling the injured part only and use caution if moving the person.
Cold:
Indirectly cool the part using ice for up to 20 minutes.
Elevate:
Only elevate the part if it does not cause more pain.
If person is experiencing:
The skin is the body’s largest organ. A burn is an injury to this organ, the skin. Burn treatments vary based on the severity of the injury.

A first degree burn affects only the uppermost or outer layer of the skin. This burn causes mild redness, swelling and pain.
A second degree, or partial thickness, burn affects both the upper layer of the skin and the skin underneath it. Some specific symptoms for this burn include: redness, swelling, pain and blistering.
A third degree, or full thickness, burn is the most severe and destroys the deep layers of the skin. This can lead to numb skin and white or blackened skin.
DO NOT:
A poison is a substance that can cause injury, illness or death if it enters the body accidently or deliberately. Some poisons are harmful if you breathe or swallow them, while others are harmful upon direct contact.

These poisons enter the body by swallowing and can include: food, drugs, alcohol, household and cleaning products, pesticides, plants and more. Some substances may not be poisonous if taken in a small quantity.

A person can also be poisoned by breathing in poison, like certain fumes and gases. Examples include: carbon monoxide (car exhaust), carbon dioxide (from sewers, wells), chlorine (found in swimming pools), glues and paints.
These poisons are absorbed through the skin, and include: plants (poison ivy, poison oak and poison sumac), fertilizers, pesticides and more.
An injected poison enters the body through bites or stings of insects, spiders, ticks, snakes and / or through medical hypodermic needles.
Activate EMS (Call 9-1-1) and call the National Poison Control Center at 1-800-222-1222. Follow dispatcher instructions. Gather the following information and inform poison control of what you learn:
Register, complete your quiz and have your personalized certification card in your mailbox!

Takes less than 2 minutes to sign up.
This username was already taken. If this is your username, you can click here to login to your existing account
Chapter 11: A sprain is the tearing of the ligaments at a joint. Use the RICE method when dealing with a sprain or strain.